Modern Medicine vs Herbal Medicine
Modern medicine or herbal medicine? Discover the science, history, and lifestyle approaches to health and healing.

In a world where a single pill can treat a symptom within hours, it’s easy to forget that humans have been harnessing the power of plants for millennia.
Modern medicine dazzles with precision, clinical trials, and lab-bench breakthroughs, while herbal medicine carries the weight of centuries of observation, ritual, and cultural wisdom.
At first glance, these two worlds might seem at odds — one focused on molecules, the other on roots, leaves, and traditions. Yet, a closer look reveals a fascinating convergence: both seek the same goal — restoring health and nurturing life.
The Science Behind Modern and Herbal Medicine
Modern medicine and herbal medicine stem from different scientific traditions, yet both share a common goal: restoring health and preventing disease.
In terms of modern medicine, it is centred around biochemical mechanisms, which refer to the specific chemical processes and interactions that occur within living organisms.
These include how cells communicate, how enzymes function, how drugs bind to receptors, how nutrients are metabolised, and how diseases alter molecular pathways. In modern medicine, understanding biochemical mechanisms enables scientists to explain precisely how a treatment works at the molecular level, predict potential side effects, and design targeted therapies.
Biochemical mechanisms are the instructions, machines, and assembly lines that keep the factory running smoothly. When a drug is introduced, it’s like adding a new tool or material that interacts with the existing system.
However, in regard to herbal medicine, it is rooted in ethnobotany, which is the scientific study of how different cultures use and understand plants, particularly for medicinal purposes, food, rituals, and daily living.
It combines anthropology and botany to document traditional plant knowledge—from Indigenous healing practices to ancient herbal systems. Ethnobotany forms the foundation of many herbal medical traditions and often guides researchers toward plants that may contain useful medicinal compounds.
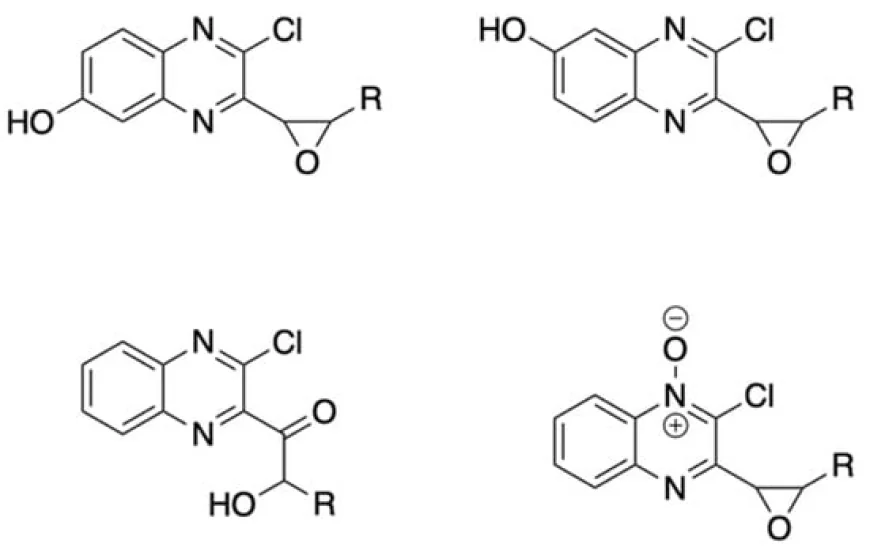
Many modern pharmaceuticals trace their origins back to plants. For example, a review of plant-based natural products notes that compounds such as salicylic acid (the precursor of aspirin), morphine, quinine, and other clinically important drugs were all originally derived from botanical sources (Newman & Cragg, 2012; Rousseaux & Schachter, 2003).
Natural-product research continues to show that a large proportion of small-molecule drugs are either directly derived from plants or inspired by plant chemistry (Newman & Cragg, 2012). Indeed, plant secondary metabolites remain a rich source of structural diversity and bioactive scaffolds for drug development.
Secondary metabolites are chemical compounds produced by plants that are not directly required for growth or reproduction, but often have important ecological or medicinal functions — for example, defence against pests, attraction of pollinators, or therapeutic effects in humans.
Many medical professionals and regulators highlight that a key barrier to wider medical endorsement of herbal products is the lack of standardisation. Herbal remedies often vary in their chemical makeup due to differences in cultivation, harvesting, and processing methods (MedCrave, 2025). Without consistent testing for active compounds, purities, and contaminants, physicians are understandably cautious about recommending them (Wang et al., 2023)
In malaria research, scientists have found that using the whole Artemisia annua plant—rather than just the single chemical artemisinin extracted from it—can sometimes be more effective in fighting malaria.
This occurs because the plant contains many different compounds that work together, a phenomenon known as synergy.
Some of these additional compounds help the drug target the parasite in multiple ways, boost the body’s immune response, or enhance the drug's absorption and distribution throughout the body.
Similarly, the other chemicals in the plant help the “main ingredient”, artemisinin, perform better, making the whole plant extract sometimes more effective than the isolated chemical alone.
Ultimately, the science behind modern and herbal medicine is not mutually exclusive. Their synergy represents a growing frontier: precision medicine informed by nature, and traditional healing guided by rigorous research. Both systems offer tools—neither is complete on its own, but they are profoundly powerful together.
A History of Modern and Herbal Medicine
The history of medicine is a narrative of evolving philosophies, discoveries, and cultural beliefs.
Herbal medicine, the oldest form of healthcare, dates back tens of thousands of years.
Archaeological findings reveal medicinal plants buried with Neanderthals. Ancient civilisations—from China and India to Egypt and Greece—developed extensive materia medica cataloguing hundreds of botanicals. These formed the backbone of Ayurveda, Traditional Chinese Medicine (TCM), and Greco-Arabic Unani systems.
Scientific research also supports this: humans have used plants medicinally since prehistoric times, long before writing existed, passing down knowledge orally through generations.
Texts such as the Ayurvedic Charaka Samhita and the Chinese Shennong Bencao Jing reveal sophisticated knowledge of physiology, energetics, and herbal synergy, long before modern laboratories existed.

A physician preparing an elixir, from an Arabic version of Dioscorides's pharmacopoeia, 1224
Modern medicine, by contrast, rapidly developed during the Scientific Revolution. The invention of the microscope in the 17th century unveiled a hidden world of cells and microbes.
Regarding germ theory in the 19th century, medicine shifted from humoral concepts to pathogen-based explanations for disease.
For example, Ancient medicine (e.g., Greek, Roman) believed that health depended on the balance of four bodily “humours”: blood, phlegm, yellow bile, and black bile. Disease was thought to result from an imbalance of these humours.
However, modern medicine understands that many diseases are caused by specific microorganisms (like bacteria, viruses, fungi) rather than imbalances in bodily fluids. This approach is based on germ theory.
Florence Nightingale’s work on sanitation, Pasteur’s vaccines, and Fleming’s discovery of penicillin fundamentally transformed the trajectory of global health.
Yet herbal medicine continued to influence this evolution. Many modern drugs were isolated from plants used traditionally. Much of early pharmacology was simply an attempt to understand how herbs worked. When chemists isolated morphine from opium poppy or salicin from willow bark, they were formalising knowledge that healers had used for millennia.
The 20th century brought industrialisation of medicine. Synthetic chemistry, randomised controlled trials, and regulatory agencies standardised treatment and improved safety.
However, this shift also distanced mainstream healthcare from holistic and plant-based practices. Herbalism became categorised as “alternative,” although it never disappeared—especially in Asia, Africa, and Indigenous communities.
By the late 20th and early 21st centuries, a renewed interest in holistic wellness led to a resurgence of herbal practices in Western societies. Integrative medicine now combines conventional treatments with safe, evidence-supported herbal remedies.
The history of modern and herbal medicine is therefore not a story of conflict, but of divergence and reconvergence. Each system preserves unique wisdom: one rooted in centuries of cultural experience, the other in scientific precision. Their shared evolution continues to shape how societies understand health.
Lifestyle, Culture, and the Spiritual Dimensions of Medicine

Beyond physiology and pharmacology, medicine is profoundly shaped by culture, lifestyle, and spirituality.
People do not choose treatments solely for biochemical reasons—they also choose based on identity, belief, and worldview.
Herbal medicine, in particular, carries cultural symbolism, while modern medicine often represents technological mastery and scientific authority.
Psychiatrists observe how cultural narratives influence patient choices.
Research shows that many people with mental‑health concerns turn to herbal or complementary medicine because they feel conventional medicine fails to address their spiritual or emotional distress. As Kelwala and Winker (2001) explain, involvement with alternative therapies often reflects a deeper “cultural paradigm” about health, spirituality, and meaning.
Complementary and Alternative Medicine (CAM) encompasses a broad range of health practices that diverge from conventional Western medicine. This includes herbal remedies, acupuncture, meditation, yoga, naturopathy, and other complementary and alternative therapies.
Unlike conventional treatments that often focus on targeting a specific disease or symptom with drugs or surgery, CAM emphasises treating the whole person — mind, body, and spirit — and often incorporates lifestyle, diet, and spiritual practices into the healing process.
Research shows that many people turn to CAM because they feel conventional medicine does not fully address their emotional, psychological, or spiritual needs.
For example, patients with mental health concerns may seek herbal medicine, meditation, or yoga because these therapies offer a sense of control, personal connection, and meaning in their treatment (Kelwala & Winker, 2001)
This reflects a broader trend: many individuals seek healing approaches that address mind, body, and meaning simultaneously.
Monastic traditions offer another dimension. In Tibetan and Zen monasteries, herbs, diet, meditation, and breathwork have long been intertwined.
In Amazonian medicine, one healer described herbs as their “teachers,” saying, “they cure you, they heal you, … they teach you … I have a lot of trust in them” (PLOS Global Public Health, 2025).
Here, herbs are part of a holistic path that emphasises awareness, compassion, and balance.
Similarly, in Ayurvedic and yogic traditions, herbal treatments are integrated with lifestyle practices, including daily routines (dinacharya), pranayama, and meditation.
As some modern Ayurvedic physicians note, “dinacharya … diet … yogasana … pranayama” are just as integral to a healing regimen as herbs (Verma et al., 2024)
Modern medicine, although historically focused on pathology rather than spirituality, is increasingly acknowledging the influence of lifestyle and mindset on health. Lifestyle-related illnesses—diabetes, heart disease, stress disorders—highlight the importance of behavioural change. Clinical research now demonstrates the therapeutic value of mindfulness, exercise, sleep, hygiene, and nutrition.
Another example of how lifestyle is entwined with herbal remedies is when someone drinks ginger tea for digestion or uses holy basil to reduce stress; they’re engaging in a cultural practice as much as a biochemical one.
Ultimately, lifestyle and culture shape how people interact with both modern and herbal medicine. Spiritual traditions remind us that healing is not only about treating disease but about cultivating connection—to nature, to community, and to oneself. As these worlds converge, the future of medicine may lie in honouring both scientific understanding and human experience.
Pain
Modern painkillers such as ibuprofen, paracetamol, and opioids act quickly and predictably by targeting inflammation or blocking pain pathways, but their potency brings risks: long-term use can lead to stomach irritation, liver stress, or dependence (as seen particularly with opioids).
On the herbal side, compounds like curcumin (from turmeric) have been shown in randomised clinical trials to reduce pain in osteoarthritis and lower inflammation biomarkers (e.g., C-reactive protein, TNF-α) with an excellent safety profile.
Similarly, willow bark extract, which contains salicin (a precursor to aspirin), has demonstrated pain relief in controlled trials for osteoarthritis.
Devil’s claw (Harpagophytum procumbens) has also been reviewed for osteoarthritis; although the data quality is mixed, some trials suggest that it can reduce pain with fewer side effects than non-steroidal anti-inflammatory drugs (NSAIDs).
Herbal approaches thus offer a gentler, longer-term strategy to support the body’s inflammatory balance—but because their effects build more slowly, they often suit chronic, mild pain better than the acute, high-intensity pain for which modern painkillers are traditionally used.
Anxiety & stress
Modern medicine often treats anxiety with drugs like SSRIs and benzodiazepines, which can quickly reduce symptoms by changing brain chemistry.
However, long-term use of benzodiazepines carries real risks: dependence, withdrawal syndrome, rebound anxiety, and other side effects.
Studies show physiological dependence can develop, and stopping suddenly may provoke a withdrawal syndrome with symptoms like increased tension, sleep issues, and panic.
By contrast, herbal remedies such as lavender and chamomile offer a gentler way to support relaxation and stress regulation.
Clinical trials have shown that inhaling lavender or chamomile essential oil can reduce anxiety scores in older adults.
Meanwhile, in studies of naturopathic care, the herb ashwagandha (Withania somnifera) was used alongside lifestyle changes and significantly reduced anxiety in people with moderate-to-severe symptoms.
Chronic illnesses - Diabetes, Arthritis, Heart Disease
Modern medicine treats chronic illnesses with well-validated drugs such as metformin for diabetes, statins for high cholesterol, and biologics for autoimmune disorders—therapies proven to improve long-term outcomes but often requiring lifelong use and carrying potential side effects.
Certain herbs show promising complementary benefits. Meta-analyses suggest that cinnamon can modestly lower fasting glucose and HbA1c levels in individuals with type 2 diabetes, although the study quality varies.
Berberine has demonstrated glucose-lowering effects comparable to those of metformin in some trials. Additionally, Boswellia serrata has been shown to reduce pain and inflammatory markers in studies of osteoarthritis.
However, these herbal therapies generally lack the potency, consistency, and large-scale evidence needed to replace standard treatment.
Their safest and most effective role is as adjuncts—supporting blood sugar control, inflammation management, and overall metabolic health when combined with medical supervision, nutrition, and lifestyle changes.

Final Thoughts
Modern and herbal medicine may speak different languages; one offers the rigour of laboratory-tested molecules, the other the richness of holistic, centuries-old knowledge.
Together, they illustrate that health is more than symptoms and prescriptions — it is a tapestry woven from science, lifestyle, and culture.
By honouring both the precision of modern pharmacology and the wisdom of plants and traditions, we can move toward a future where medicine is not just about curing disease, but about nurturing the whole person — mind, body, and spirit.


